New clues point to the microbiome.

In clinics from Boston to Brisbane, doctors keep hearing the same odd pairing: mood symptoms and stomach problems arriving together. For years it was treated as coincidence or stress. But newer research is tightening the story. The gut is not just digestion, it is hormones, immune signals, and trillions of microbes producing chemicals that reach the brain. The surprise is how often small shifts in that internal ecosystem line up with anxiety, depression, and brain fog.
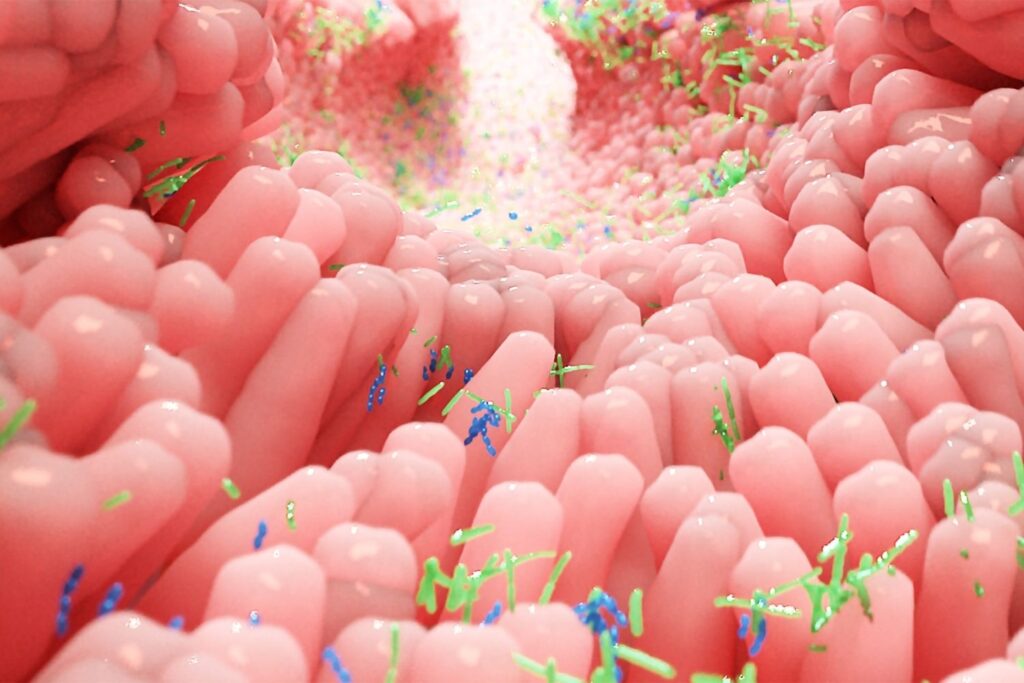
1. The microbiome may influence mood chemistry daily.

The gut microbiome is a chemical factory that runs around the clock. As bacteria digest fiber and other nutrients, they produce metabolites that can enter the bloodstream and influence inflammation and neurotransmitter pathways. When those microbial communities shift, the chemical output shifts too, and mood can follow.
Some of the strongest evidence comes from metabolites called short chain fatty acids, which are linked to immune regulation and brain signaling. Changes in these compounds show up repeatedly in depression research, including in human and animal studies, according to a 2024 review in PubMed Central. That does not mean bacteria control emotions like a switch, but it does suggest mood is partly downstream of biology happening far below the ribcage.
2. Inflammation from the gut can reach the brain.
When the gut barrier is stressed, fragments of bacteria and inflammatory molecules can leak into circulation. The immune system reacts, and that reaction can influence brain function through cytokines that alter neurotransmitter activity and stress responses. This is one reason depression is increasingly studied as partly an inflammatory condition for some people.
The clue is that certain microbial patterns appear tied to immune activation in ways that correlate with depressive symptoms. A recent Harvard Medical School report described research linking specific gut bacteria to inflammation pathways connected with major depressive disorder, as reported by Harvard Medical School News. It is not a simple cause and effect for everyone, but the immune route offers a plausible bridge between digestion and mood shifts that feel unexplained.
3. The vagus nerve may carry gut signals upward.
The vagus nerve is like a fast communication line between the gut and the brainstem. It responds to stretch, hormones, and immune activity in the digestive tract, and it can influence stress regulation, heart rate variability, and emotional reactivity. When gut conditions change, vagal signaling can change with them.
This matters because the vagus does not require bacteria to travel anywhere. It translates gut conditions into nerve messages in real time. Researchers reviewing serotonin signaling and vagal pathways note that microbial metabolites can influence serotonin production and vagal activity, shaping gut brain communication, as stated by a 2025 review in PubMed Central. It helps explain why nausea, dread, and calm can feel physically linked.
4. Stress can reshape gut microbes surprisingly fast.

Stress hormones change digestion, blood flow, and gut motility, and those shifts can change which microbes thrive. Even short periods of disrupted sleep or chronic anxiety can alter eating patterns and gut transit time, which can shift microbial balance. This creates a feedback loop where stress changes the gut, and the gut may then influence stress resilience.
In practical terms, this can look like anxiety that worsens during high pressure weeks, paired with bloating or irregular digestion. The biology is not just psychological. The body is adjusting to threat mode and the gut ecosystem adapts to that environment. Over time, a stressed gut may produce fewer helpful metabolites and more inflammatory signals, making emotional recovery feel slower than it should.
5. Food patterns can change mental clarity over weeks.

Diet is one of the strongest levers on the microbiome because it decides what microbes are fed. High fiber diets tend to support a wider range of bacteria that produce beneficial metabolites, while low fiber and high ultra processed patterns can narrow diversity and shift chemistry. Those changes do not stay confined to digestion.
People often notice it first as brain fog or irritability rather than stomach pain. A diet shift can also affect blood sugar swings, which influence anxiety sensations like racing heart and shakiness. What makes this area tricky is that diet effects are slow and personal. Still, consistent patterns show that food can alter microbial output, immune tone, and energy regulation in ways that shape mood without needing a dramatic trigger.
6. Antibiotics can leave emotional ripples afterward.

Antibiotics can be lifesaving, but they also reduce microbial populations quickly, including bacteria that help regulate inflammation and metabolite production. After a course, the gut may repopulate unevenly, and some people notice digestive disruption paired with mood changes. The timing can feel suspicious, like an emotional shift that starts after a medical event.
This does not mean antibiotics cause depression broadly, but they can change the conditions that support stable mood for certain individuals. Reduced microbial diversity can temporarily lower production of short chain fatty acids and other compounds involved in immune balance. For people already vulnerable due to stress or sleep loss, that microbial shock can add another layer of strain, and the mind may register it as anxiety, restlessness, or low motivation.
7. Sleep loss can disturb gut rhythms at night.

The gut has its own daily rhythm. Motility, hormone release, and microbial activity shift across the day and night, and sleep disruption can scramble that timing. Late nights and irregular schedules can change when you eat, how your gut moves, and which microbes dominate at certain hours.
This matters because circadian disruption is already linked to mood disorders, and the gut may be one reason. When the digestive system is out of sync, inflammation can rise and glucose control can worsen, both of which affect mental steadiness. People often blame the mind alone, but the gut is also reacting to an off schedule body. The result can be a morning that feels anxious and wired, even when nothing stressful is happening externally.
8. Some probiotics help, but results vary widely.

Probiotics are often marketed like universal fixes, but microbiome science suggests their effects depend on the starting ecosystem. A strain that benefits one person may do nothing for another. Some strains may influence gut barrier function or reduce inflammation, but the clinical evidence is mixed and often modest.
The more realistic view is that probiotics can be one tool, especially after antibiotics or digestive illness, but they are not a replacement for mental health care. Diet, sleep, and stress regulation still matter more consistently because they shape the environment microbes live in. If probiotics help, it is often by nudging immune balance and metabolite production rather than directly creating happiness. The benefits can be subtle, like steadier energy, fewer stress stomach flares, or improved sleep onset.
9. Gut sensitivity can make anxiety feel physical first.

Many people experience anxiety as a body sensation before a thought. Tight chest, nausea, cramps, or a sudden urge to use the bathroom can arrive first, then the mind scrambles to explain it. The gut is packed with nerves and serotonin receptors, making it a highly reactive organ during stress.
When gut motility speeds up, the body can interpret it as threat. That sensation can spiral into worry, even if the trigger was a meal, caffeine, or inflammation. This is why gut focused care sometimes reduces anxiety symptoms without changing a persons life circumstances. Calming the digestive system can lower the volume on bodily alarms, making the brain less likely to interpret normal sensations as danger. It is a pathway of perception, not weakness.
10. Future treatments may target microbial metabolites directly.
The most interesting shift is that researchers are moving beyond naming bacteria and toward tracking what bacteria produce. Metabolites like short chain fatty acids, bile acid derivatives, and tryptophan related compounds may be more actionable than chasing specific species. If you can measure a metabolite profile, you can design interventions that restore balance more precisely.
This could lead to new diagnostics that flag risk earlier, especially for people with treatment resistant depression or chronic anxiety paired with digestive symptoms. It may also reshape psychiatric care toward integrated models where gut health is evaluated alongside sleep, inflammation markers, and stress physiology. The gut may not replace therapy or medication, but it may become a standard part of the workup, changing how mental health is treated in everyday clinics.
